Bioethical Issues: Bioethics refers to the study and evaluation of the decisions done in scientific research and medicine to touch upon the health and lives of people, as well as the society and environment. Bioethics is a portmanteau of the words “bio” and “ethics“.
Because of that, this discipline is concerned about determining the rightness or wrongness of the discoveries and developed technologies in science, as well as incorporating human rights and values to health and life.
The following topics are the most common scientific topics and advancements that have gotten the attention of bioethics supporters, the media, and the general public.
Table of Contents
- Top Bioethical Issues
- 1. Abortion
- 2. Surrogacy
- 3. Whole Genome Diagnosis
- 4. Cloning
- 5. Stem Cells
- 6. Eugenics
- 7. Genetically Modified Organisms
- 8. Healthcare
- 9. Aged Care
- 10. Euthanasia
- 11. Organ Donation
- 12. Head Transplant
- 13. Cryonics
- 14. Bone Conduction
- 15. Precision Medicine
- 16. Neuroethics
- 17. Artificial Intelligence in Healthcare
- 18. Digital Health Data and Privacy
- 19. Biosecurity and Dual-use Research
- 20. Animal Rights in Research
- 21. Nanomedicine
- 22. Biobanking
- 23. Artificial Exoskeleton
Top Bioethical Issues
1. Abortion

Abortion refers to the premature ending of a pregnancy which occurred in itself (known as a miscarriage or spontaneous abortion) or by force through surgery or taking medications. The topic of abortion raises intensely personal issues about many topics, such as morals, religion, sexuality, autonomy, politics, and science and medicine.
- During the abortion, the central question is focused on whether or not unborn children (called fetuses) have moral status and significance. Aside from that, questions regarding parental responsibilities and obligations and the issue of personhood arise.
- Although abortion has long been debated in almost all issues in bioethics, there is still no moral consensus achieved.
![]()
2. Surrogacy

The next bioethical issue in our list is Surrogacy. Surrogacy assists the reproduction of parents who are incapable of doing so (e.g., same-sex couples, single men, single women, or man/wife). Most of the time, surrogacy is carried out by women (known as gestational women or gestational surrogate) who carries the child in their womb.
- The bioethical concern here is the confusion in the identity of the child, whether or not his biological parents are considered his “true” parents.
![]()
3. Whole Genome Diagnosis
Advancements in technology are now able to allow researchers and physicians to view and have access to the whole genome of a newborn. Such screening is used to determine the individual’s chances of acquiring and developing certain diseases.
- However, this process seems to draw criticisms primarily because of the lack of consent from the individual (a.k.a the newborn).
![]()
4. Cloning

Cloning refers to the process of creating a new population of genetically-similar and identical naturally occurring organisms. The usual targets for cloning include bacteria, plants, and animals.
- In particular, the bioethical issues regarding cloning focus on humans becoming the subject of such experiments.
- The moral status of the cloned organism, created mainly for destruction and as a source of organs, has become the primary concern in bioethics. Issues include health risks to both mother and child, damage to the clone, meager success rates even if there are a lot of trials and samples, psychological effects to the clone, and commodification and commercialization of life itself. Refer to pros and cons of cloning here.
![]()
5. Stem Cells

In biology, stems cells are a type of undifferentiated (not mature and undeveloped) cells that can divide and differentiate into specialized cells.
- The bioethical issue concerning stem cells is pretty much like the issues with cloning.
- Respect for life per se requires that people show respect to all of its forms. Supporters of bioethics believe that stem cell research violates this notion because the source organism (usually an embryo) is destroyed during the process.
- While stem cell research can alleviate human diseases and suffering, creating stem cell lines may lead to the uncontrolled commodification of cells and life.
![]()
6. Eugenics
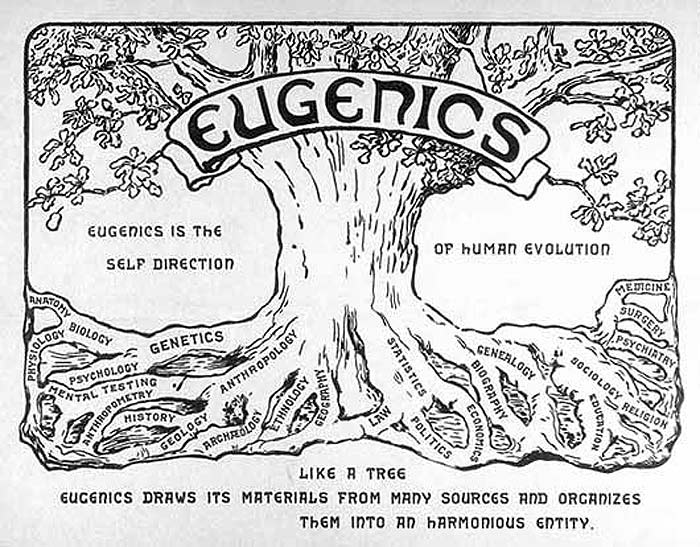
In philosophy, eugenics refers to the social movement that believes on the possibility of creating the best human society and race by promoting the reproduction of populations with positive or desirable traits while controlling and prohibiting the reproduction of populations with negative or undesirable traits.
- Eugenics became very popular when Adolf Hitler ordered the killing of disabled and medically unfit people as well as the murdering of the Jews.
- Because of the advancement of science and technology, many people fear that another era where the principle of genetics will prevail. Ethical issues about eugenics concern the moral principle associated with racial equality and the subjective belief in perfection.
![]()
7. Genetically Modified Organisms
GMOs, or genetically modified organisms, are organisms that have been transplanted with a gene or a DNA sequence of interest from another organism. This process is similar to eugenics, wherein an organism with the best traits is produced.
- However, unlike eugenics, the process of creating GMOs requires work on the genetic level and is usually done in crops and animals.
- While the production, use, and creation of genetically modified organisms are new, with their long-term impacts on health still yet to be seen, bioethical issues about it are the same with cloning, stem cell research, and eugenics.
![]()
8. Healthcare

As alluded to earlier, several technological advancements have paved the way for the improvement in health care.
- Aside from that, issues regarding the allocation of funds, decision-maker and recipient of the benefit, cost-efficiency, and measurement of success are ethical concerns. Aside from that, many people believe that health care may only promote health inequality.
![]()
9. Aged Care

A portion of the world’s population is composed of elderly citizens. Naturally, they become the priority for funding and public policy through aged care establishments and other accommodation services.
- However, similar to health care, these policies raise concerns about who should provide support for the elderly and what should be their standards of living.
- In addition to that, questions about balance, freedom, and safety are also being asked.
![]()
10. Euthanasia

Literally meaning “good death“, euthanasia is the process of intending to end the life an individual to stop their pain and suffering. Euthanasia is also loosely called mercy-killing, assisted suicide, or doctor-assisted suicide.
- While some people believe that euthanasia is just a matter of ending life painlessly, many people (especially those who support bioethics) believe otherwise.
- In many countries, euthanasia is illegal, regardless of the circumstances.
- Euthanasia challenges the belief about the sanctity and equality of all life forms. Euthanasia is believed to corrupt the practice of medicine and undermine the value of suicide prevention.
![]()
11. Organ Donation
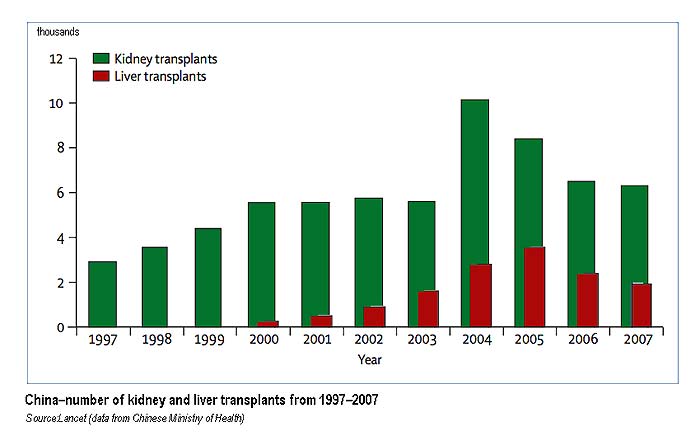
Despite being almost common, donating or receiving an organ raises ethical issues. Similar to cloning and stem cell research, organ donation have raised numerous moral, societal, and ethical concerns about the use of living people as donors.
- The first bioethical issue on organ donation is a big shortage of organs for those who need them. There are thousands of people on the waiting list to receive organ transplants, either living or deceased. Check out United Network for Organ Sharing (UNOS) for the updated waiting list, statistics around how many people are being added to the list per minute, how many people are getting the transplant and how many people die every day during the transplant surgeries & more.
- The next bioethical issue on this matter is equal access to organs (aka distributive justice theory) to those who need them by the length of waiting time and by their age. According to this theory, the patients who wait for transplants could not move up the waiting list if their poor lifestyle caused damage to organs (like smoking or substance abuse) over patients who have no control over their diseases.
- Another biggest ethical issue is that as there is a big demand for organ transplants, there is a fear of illegal organ stealing from livings (human trafficking) without their consent to create organ farming to sell body parts for high prices.
![]()
12. Head Transplant
Absurd as it may sound, experiments about transplanting an organism’s head to another are being done. In fact, during the 1970s, the first-ever head transplant in monkeys occurred successfully (the recipient only lived for ten days).
- While such application on humans is still being studied, serious health and bioethical concerns are associated with it. Questions like the brain’s reaction to the new body, memory, and individual identity, are of concern.
![]()
13. Cryonics
Cryonics refers the scientific method of freezing a newly-dead individual to reanimate or bring him to life at a later period. Because this process involves reversing the process of death, several bioethical issues were raised against it.
- One of the main problems with cryonics is immortality. While some believe immortality to be beneficial, bioethics supporters believe this idea should not prevail, given that the planet is already under a crisis of unsustainable population and limited resources.
![]()
14. Bone Conduction
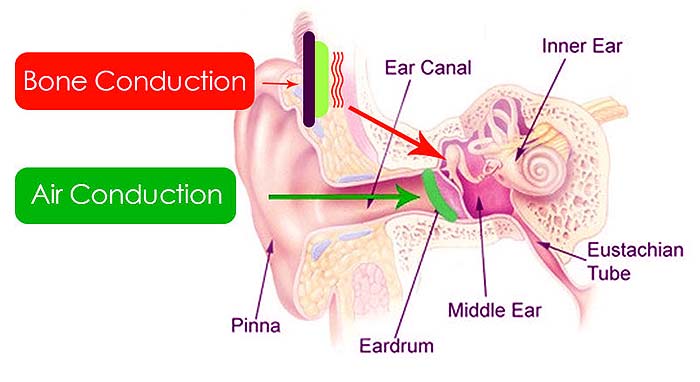
Bone conduction technology involves the replacement of an individual’s ear bones to transducers that can transmit sounds.
- Despite being promising, the problem with this technology is that it can transform an individual into a billboard with countless advertisements. In this case, the consent of the individual is not a concern.
![]()
15. Precision Medicine
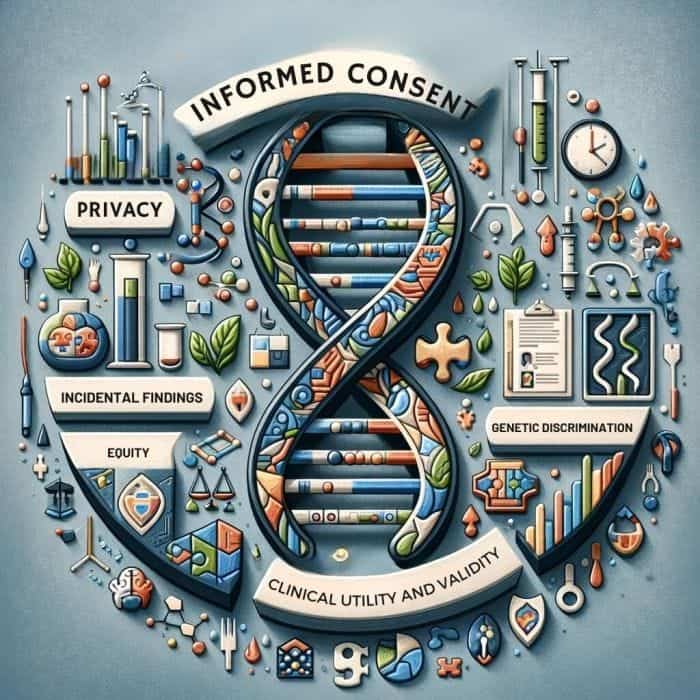
Precision medicine represents a tailored approach to healthcare, where medical decisions, treatments, and practices are customized to the individual patient based on their genetic, environmental, and lifestyle factors. This innovative approach aims to optimize efficiency and outcomes by focusing on the individual characteristics that influence health and disease.
However, the implementation of precision medicine raises several ethical challenges:
- Informed Consent: Ensuring patients have a comprehensive understanding of what their genetic data will be used for, potential risks, and the implications of uncovering unknown genetic information.
- Privacy and Data Security: Protecting the sensitive genetic and health information collected in precision medicine from unauthorized access or breaches, addressing concerns over privacy and confidentiality.
- Equity: Addressing disparities in access to precision medicine technologies and treatments to prevent exacerbating healthcare inequities among different populations and socioeconomic groups.
- Incidental Findings: Managing the discovery of incidental findings that could have significant implications for the patient or their family members’ health and deciding how these findings should be communicated.
- Genetic Discrimination: Preventing discrimination based on genetic information, particularly by employers or insurance companies, ensuring that individuals are not unfairly treated because of their genetic predispositions.
- Clinical Utility and Validity: Evaluating the effectiveness and reliability of precision medicine interventions and ensuring they genuinely improve patient outcomes before widespread adoption.
- Ethical Use of Genetic Information: Navigating the ethical considerations around genetic information in healthcare decisions, including reproductive choices and disease prevention strategies.
These challenges require careful consideration and the development of ethical frameworks and policies to guide the responsible use of precision medicine, ensuring that advancements in healthcare are accessible, equitable, and respectful of patient rights and privacy.
![]()
16. Neuroethics
Neuroethics is an interdisciplinary field that explores neuroscience’s ethical, legal, and social implications. It examines how advancements in understanding the brain and mind influence our notions of self, agency, morality, and social fabric. Neuroethics addresses the consequences of applying neuroscientific knowledge and technologies to cognitive enhancement, mental health, criminal responsibility, and privacy.
The ethical considerations in neuroethics include:
- Cognitive Enhancement: Debating the ethical use of pharmaceuticals or technologies to improve cognitive function in healthy individuals, including concerns about coercion, fairness, and societal pressure.
- Mental Privacy and Consent: Protecting individuals’ right to mental privacy against technologies that could potentially read or influence thoughts and ensuring informed consent in using such technologies.
- Neurotechnology and Autonomy: Examining the impact of brain-computer interfaces and other neurotechnologies on personal autonomy, identity, and the essence of human experience.
- Mental Health and Stigma: Addressing ethical issues in diagnosing and treating mental health conditions, including the potential for increased stigma or misunderstanding of mental health.
- Brain Research and Vulnerable Populations: Ensuring that brain research does not exploit vulnerable populations and that all research participants are treated with respect and dignity.
- Free Will and Moral Responsibility: Investigating how neuroscientific insights into Human Behavior impact concepts of free will, moral responsibility, and the legal system.
- Data Privacy in Brain Imaging: Safeguarding the privacy of data obtained through brain imaging and ensuring that such data is used ethically and responsibly.
As neuroscience continues to unveil the complexities of the brain and mind, neuroethics plays a critical role in guiding the responsible use of these discoveries, ensuring that advancements benefit society while respecting individual rights and dignity.
![]()
17. Artificial Intelligence in Healthcare

Integrating Artificial Intelligence (AI) in healthcare promises to revolutionize diagnosis, treatment, and patient care. AI technologies, including machine learning algorithms and deep learning networks, have the potential to analyze complex medical data, improve diagnostic accuracy, personalize treatments, and predict patient outcomes.
However, the deployment of AI in healthcare also raises substantial ethical considerations:
- Bias and Fairness: Addressing biases in AI algorithms that could lead to unequal treatment or outcomes for certain patient groups, particularly if the data used for training AI models does not represent diverse populations.
- Transparency and Explainability: Ensuring that AI-based decisions can be understood and interpreted by healthcare providers and patients, given the “black box” nature of some AI systems.
- Patient Consent and Privacy: Safeguarding patient privacy and confidentiality in the use of AI, including informed consent about how AI is used in their care and how their data contributes to AI training.
- Clinical Validation and Safety: Validating the safety and effectiveness of AI applications in healthcare through rigorous testing and clinical trials to ensure they meet high standards of patient care.
- Autonomy and Human Oversight: Balancing the benefits of AI with the need for human oversight in clinical decision-making, preserving the autonomy of healthcare professionals and patients in treatment decisions.
- Equity of Access: Preventing disparities in access to AI-enhanced healthcare services, ensuring that advancements in AI benefit all individuals equally without widening existing healthcare gaps.
- Liability and Accountability: Clarifying legal and ethical responsibility for AI-driven healthcare decisions, especially in cases of diagnostic errors or treatment failures.
Tackling these challenges demands teamwork from ethicists, technologists, clinicians, patients, and policymakers to guarantee AI’s ethical, responsible development and implementation in healthcare, prioritizing patient well-being.
![]()
18. Digital Health Data and Privacy
The rise of digital health technologies, including electronic health records (EHRs), wearable devices, telehealth, and health apps, has transformed healthcare delivery and management. These technologies facilitate the collection, storage, and analysis of vast amounts of health data, enabling advancements in personalized medicine, disease tracking, and health outcomes research.
However, the digitization of health information also introduces significant ethical challenges related to data privacy and security:
- Data Privacy and Protection: Ensuring the confidentiality and security of digital health data against unauthorized access, breaches, and cyberattacks.
- Informed Consent: Obtaining clear and informed consent from patients for the collection, use, and sharing of their digital health data, with transparent information about potential uses.
- Data Ownership and Control: Clarifying the rights of individuals over their health data, including access, control, and the ability to correct inaccuracies or request data deletion.
- Secondary Use of Data: Addressing ethical considerations around the secondary use of health data for research or commercial purposes beyond the original consent use.
- Regulatory and Ethical Frameworks: Developing and adhering to robust ethical and legal frameworks that protect individuals’ rights and ensure responsible use of digital health data.
- Transparency and Accountability: Maintaining transparency in data collection, processing, and sharing practices and holding entities accountable for data misuse or ethical breaches.
Addressing these ethical challenges is key to preserving trust in digital health technologies and ensuring healthcare digitization’s advantages are achieved ethically and fairly.
![]()
19. Biosecurity and Dual-use Research
Biosecurity and Dual-use research involve scientific work that has the potential to be used for both beneficial and harmful purposes. This dual-use nature raises significant ethical challenges, as the same technologies that can lead to major advancements in fields such as medicine, agriculture, and environmental protection can also be misused in ways that threaten public health, national security, and global stability.
The ethical dilemma lies in fostering scientific innovation and sharing knowledge while preventing the misuse of research findings, technologies, or biological agents that could lead to the development of biological weapons or facilitate bioterrorism. These concerns necessitate carefully considering how to conduct and disseminate research responsibly, ensuring that the benefits of scientific discoveries are realized without compromising biosecurity. Key ethical issues in biosecurity and dual-use research include:
- Assessment of Risks and Benefits: Weighing the potential scientific and public health benefits of research against the risks of its misuse.
- Responsibility and Oversight: Defining the responsibilities of researchers, institutions, and policymakers in regulating and overseeing dual-use research to minimize risks.
- Transparency vs. Secrecy: Striking a balance between the scientific norm of openness and the need to restrict certain information to prevent misuse.
- Regulation and Governance: Developing international and national governance frameworks that effectively manage dual-use risks while supporting scientific progress.
- Education and Awareness: Enhancing awareness among scientists, policymakers, and the public about the dual-use potential of scientific research and the importance of ethical conduct.
![]()
20. Animal Rights in Research
The use of animals in research is a critical area of ethical concern that balances the pursuit of scientific knowledge and medical advancements with the welfare and rights of animals. This area of bioethics addresses the moral implications of utilizing animals for experimental purposes, focusing on minimizing harm and ensuring humane treatment.
Ethical considerations in animal research include:
- Necessity and Justification: Evaluating the scientific necessity of using animals in research and ensuring the potential benefits justify the ethical costs.
- Three Rs Principle: Adherence to the principles of Replacement (using non-animal alternatives whenever possible), Reduction (minimizing the number of animals used), and Refinement (employing methods that reduce suffering and improve animal welfare).
- Welfare and Humane Treatment: Ensuring the highest animal welfare standards, including proper housing care and minimizing pain and distress through appropriate use of anesthesia and analgesia.
- Ethical Review and Oversight: Subjecting research proposals to rigorous ethical review by institutional committees to evaluate the ethical justification for animal use, the application of the Three Rs, and the welfare considerations.
- Transparency and Responsibility: Maintaining transparency about the use of animals in research and researchers’ responsibility for the ethical treatment of their animal subjects.
- Public Engagement and Education: Engaging with the public about the ethical dimensions of animal research, the benefits of such research for human and animal health, and the measures taken to ensure ethical conduct.
- Regulatory Compliance: Complying with national and international laws, guidelines, and standards that govern the ethical use of animals in research.
These ethical issues require a balanced approach that respects the intrinsic value of animal life while recognizing the potential benefits of research for understanding diseases, developing new treatments, and improving human and animal health.
![]()
21. Nanomedicine
Nanomedicine, the application of nanotechnology in healthcare, offers revolutionary opportunities for diagnosing, preventing, and treating diseases. It encompasses a broad range of technologies, including drug delivery systems, diagnostic techniques, and regenerative medicine, utilizing nanoparticles and nanostructures to achieve precise interactions at the molecular and cellular levels.
While nanomedicine holds promise for significantly advancing medical science and patient care, it also raises several ethical issues:
- Safety and Toxicity: Assessing the long-term safety and potential toxicity of nanomaterials in the human body, given their ability to cross biological barriers and interact at the cellular level.
- Informed Consent: Ensuring patients are fully informed about the novel aspects of nanomedicine treatments, including potential risks and uncertainties, to make educated decisions about their care.
- Equity of Access: Addressing disparities in access to nanomedicine technologies, ensuring that advancements do not widen existing healthcare inequalities.
- Privacy: Managing the implications of nanotechnology-based diagnostics and monitoring devices that could collect sensitive health data, ensuring patient privacy is protected.
- Regulation and Oversight: Developing appropriate regulatory frameworks to govern the development, testing, and use of nanomedicine products, ensuring they are safe, effective, and ethically deployed.
- Environmental Impact: Evaluating and mitigating the environmental consequences of producing and disposing of nanomaterials, considering their persistence and potential toxicity in ecosystems.
- Dual Use and Misuse: Preventing the potential misuse of nanotechnologies for purposes other than their intended medical applications, including concerns related to biosecurity and bioterrorism.
Managing these ethical considerations necessitates a collaborative effort from ethicists, scientists, regulators, and the public to guarantee nanomedicine’s development is both safe and equitable, respecting patients’ rights and dignity.
![]()
22. Biobanking
Biobanking involves collecting, storing, and managing biological samples, such as blood, tissue, and DNA, along with associated health data for use in research and medicine. While biobanks are invaluable resources for advancing medical research, personalized medicine, and understanding of diseases, they also raise several ethical issues:
- Informed Consent: Ensuring donors are fully informed about the scope of research, potential future uses of their samples, and the possibility of unforeseen findings to make an informed decision about participation.
- Privacy and Confidentiality: Protecting the personal and health information associated with biological samples against unauthorized access and ensuring donors’ privacy and confidentiality.
- Ownership and Control: Clarifying the ownership of biological samples and associated data and determining who has control over their future use, including the rights of donors to withdraw consent.
- Benefit Sharing: Addressing how benefits arising from research using biobank materials, such as new treatments or discoveries, are shared with donors, communities, and society.
- Return of Results: Determining policies for if and how individual research or incidental findings may have clinical significance are communicated to donors.
- Equity and Access: Ensuring equitable access to the benefits of research conducted with bio-banked materials and preventing exploitation of specific groups or communities.
- Transparency and Trust: Maintaining transparency in biobanking operations and research use of samples to build and maintain trust with donors and the public.
Navigating these ethical issues in biobanking requires careful consideration and balance between the potential benefits of biobanks for research and medicine and donors’ rights, privacy, and welfare.
![]()
23. Artificial Exoskeleton
The development and use of artificial exoskeletons, devices designed to enhance human physical capabilities, raise significant bioethical considerations. These wearable machines can be used for various purposes, including assisting individuals with mobility impairments, augmenting the strength of workers in physically demanding jobs, or enhancing soldier performance in military applications.
While artificial exoskeletons offer promising benefits, they also introduce ethical challenges that need to be addressed:
- Accessibility and Equity: Ensuring that the benefits of artificial exoskeleton technology are accessible to all individuals who need them, regardless of socioeconomic status, to prevent exacerbating existing health and social inequities.
- Autonomy and Consent: Respect users’ autonomy by obtaining informed consent regarding exoskeletons, including clear communication about potential risks and benefits.
- Privacy and Data Security: Addressing concerns related to collecting, using, and storing personal data by exoskeletons equipped with sensors and other data-gathering technologies.
- Enhancement vs. Therapy: Navigating the ethical boundary between therapeutic use for individuals with disabilities and enhancement uses that could lead to social pressures or unfair advantages.
- Long-term Effects and Dependence: Assessing the long-term health effects of using artificial exoskeletons, including potential physical dependency or impacts on mental health and identity.
- Regulation and Safety Standards: Developing regulatory frameworks and standards to ensure exoskeleton technologies’ efficacy, safety, and reliability.
- Liability and Responsibility: Determining liability in malfunction or injury caused by exoskeleton use, including clarifying the responsibilities of manufacturers, healthcare providers, and users.
Navigating these ethical issues requires multidisciplinary collaboration among ethicists, engineers, healthcare providers, and policymakers to ensure that artificial exoskeleton technologies are developed and used to promote human well-being and equity.
![]()
In conclusion, we can infer that even in the best-case situations, some of the aforementioned scientific methods and medical practices are a dangerous and problematic ethical minefield.















[…] Top Bioethical Issues […]