The current discovery in immunology showcases the recent development and its relevance during the upsurge in COVID-19 cases. The previous treatise (2021) describes the development of immunology as a scientific discipline focusing on immune-responsive cells, a cancer immunotherapeutic approach, the discovery of synthetic vaccines, and a way to treat asthma and other lung inflammations using macrophage populations.
Top Immunology News of 2022
1. A new study demonstrates how COVID-19 affects the gut immune system (UK, Feb 2022)
The effect of the virus on the gut immune system has been demonstrated in new research using intestine samples from persons who have died of COVID-19.
- For this purpose, samples of the gastrointestinal tract from patients who passed away after receiving a COVID-19 diagnosis were examined during the initial wave of the pandemic.
- While severe COVID-19 can cause breathing difficulties and high fever in some patients, other symptoms, including diarrhea, nausea, and vomiting, involve the gastrointestinal tract.
- According to researchers, the Peyer’s Patches system, which typically controls how the microbial communities are composed, was extensively disrupted in severe COVID-19.
- Whether or not there was evidence of a virus in the intestines had no bearing on this. Independent of the local viral levels, observations of the samples revealed that Peyer’s Patches, a collection of lymphoid follicles that borders the small intestine, had changed in structure and cellularity.
- In individuals who died from COVID-19, this included the depletion of the germinal centers, which typically multiply antibody-producing cells.
A decrease in microbial diversity, or dysbiosis, could occur from the inadequate local immunity that follows. The results also imply that oral immunization might be ineffective if the patient is already unwell due to the impaired gut immune system.
2. Researchers find out why the protective effects of malaria immunization fast wear off (Germany, June 2022)
Every year, malaria still kills more than 600,000 people worldwide, primarily due to the parasite Plasmodium falciparum. Just one vaccination has been licensed to protect against this one-celled organism, and it loses its effectiveness quickly.
- The CSP protein, which is quantitatively the most abundant on the surface of the “sporozoites, ” is the target of the vaccination.
- Sporozoites are the stage of the malaria infection that enters human blood after being bitten by a mosquito.
- It’s critical to know which protective antibodies the vaccine produces to improve it. However, the so-called follicular T helper cells play a significant role in generating these antibodies.
- They ensure that B cells develop into memory B cells and plasma cells that produce antibodies. The scientists tested the blood of participants exposed to the vaccine strain’s killed P. falciparum sporozoites to thoroughly study the T helper cell response against CSP.
- The researchers examined the induced follicular T helper cells at the single-cell level. They specifically concentrated on determining which T helper cell receptors recognize CSP sequences.
- The findings showed that the T-cell receptors mostly focused on the CSP’s amino acids 311 to 333. Also, it was discovered that there was almost little cross-reactivity between the various T-cell clones.
- The CSP epitopesWhat is epitopes?Epitopes are specific regions on an antigen that are recognized and targeted by the immune system's antibodies or cells. of the employed vaccination strain are the only ones the receptors specifically bind.
- The persistent natural infections with the pathogen do not serve as a natural “booster” because of the specificity of the T-cell clones. This may help explain why the malaria vaccine’s protective effect subsides quickly.
The researcher suggests that future research on the vaccine should examine whether stimulating a wider variety of T helper cells could result in a more robust immune response.
3. Researchers identify crucial allergic reactions to pollen from the plant mugwort (Austria, June 2022)
For those who are allergic, mugwort (Artemisia vulgaris) presents a major concern. The symptoms that frequently cause asthma can only be managed symptomatically at this time. A study team has identified crucial mechanisms behind sensitivity to pollen from the common weed mugwort, setting the groundwork for the creation of the first vaccine in history.
- The scientists began their preclinical research at the place where mugwort pollen allergies first developed.
- They discovered where and how the immunoglobulin E (IgE) type antibodies locate and activate the heightened immune response to the main mugwort pollen allergen (Art v 1).
- Also, they discovered that specific protein building blocks of the primary mugwort pollen allergen are arranged in a way that allows IgG (immunoglobulin G) antibodies to block them. These discoveries were the foundation for creating a vaccination to prevent mugwort allergies.
- The study demonstrates the potential for safe and successful treatment using fragments of the main mugwort pollen allergen.
- Observations of the vaccine’s mechanism of action reveal that one of the ends of the primary mugwort pollen allergen serves as a crucial docking site for the pathogenic IgE antibodies of allergic people, which can be utilized to develop a new vaccine.
Mugwort is common in the northern hemisphere, where from July through September, its pollen can make sensitive people feel uncomfortable and even develop asthma. The study’s findings might be applied to creating a synthetic vaccine that can be tested in a clinical trial.
4. Research on intratumoral immune responses reveals worse prognoses and outcomes of non-reproductive malignancies in males (USA, June 2022)
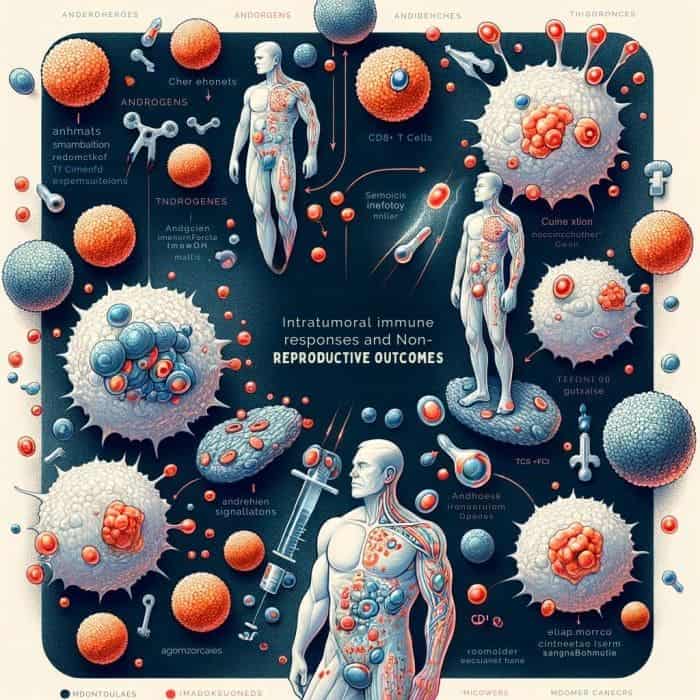
Incidence, progression, response to treatment, and survival outcomes differ noticeably across sexes in patients with malignancies originating in non-reproductive organs, such as bladder and liver cancer. Male patients typically have worse prognoses and outcomes.
- This study concentrated on the T cell immune response to malignancy, a crucial factor in cancer outcomes and a crucial target that has aided in reviving cancer immunotherapy.
- The study revealed a ground-breaking discovery that male sex hormones influence cancer-related sex bias through modulating CD8+ T cells, a population of lymphocytes often known as cancer “killer” cells.
- CD8+ T cells regulate adaptive immunity and build an antitumor response.
- Sex hormones called androgens are more prevalent in men. According to this study, CD8+ T cells from cancers in male subjects—including human cancer patients and mice—are more likely to exhibit signs of a compromised immune response against the tumor, also known as “exhausted” T cells.
- By modifying the expression of TCF1, a master regulator of CD8+ T cell activity, androgen signaling promotes the progenitor-exhausted CD8+ T cell phenotype.
Targeting this signaling cascade is key to improving cancer immunotherapies because androgen-mediated stimulation of CD8+ T cell malfunction leads to quicker tumor development and worse outcomes.
5. Study shows that cognitive behavioral therapy can help children with anxiety brought on by food allergies (USA, Oct 2022)
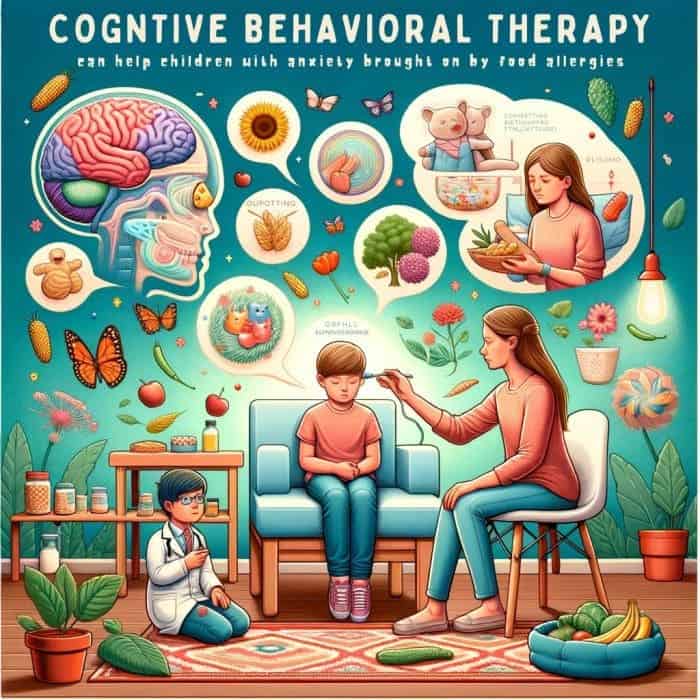
Parents and kids with food allergies frequently experience increased worry due to the potential dangers of accidental interaction with food allergens. According to a recent study, tailored cognitive behavioral therapy (CBT) can considerably reduce anxiety caused by food allergies in both children and parents.
- Participants in the study were 10 children (8–12 years old, 80% female) who had been sent by their allergists for evaluation and management of FAA.
- The children had to have medically unnecessary and impairment-causing excessive worry and nervous avoidance primarily connected to their food allergy, as well as proven IgE-mediated food allergy/allergies that were under control.
- The patient participated in 5-8 “proximity exposure sessions” as part of the CBT. Depending on whether it was a group or solo session, the length of each session ranged from 30 to 90 minutes.
- The sessions were led by an allergist or mental health professional. Each session included a range of graded exposures that the whole group participated in, such as touching or sniffing their allergen or eating a meal they would otherwise avoid or dread.
- One or both parents of each child answered a post-treatment survey about treatment satisfaction.
- Parents rated The treatment as helpful and satisfactory, and all 10 children were rated as significantly improved or very significantly improved. Despite the short sample size of only 10 kids, all the kids and their parents displayed symptom improvement.
More trials are still needed because the sample size was limited. CBT may help allergists and other experts who work with children, such as mental health specialists, in their treatment efforts. This manualized therapy only requires 6 sessions and may be administered by nurse practitioners or other healthcare professionals in allergists’ offices.
6. Research shows while certain intestinal viruses support intestinal health, others are linked to inflammatory bowel disease (USA, Apr 2022)
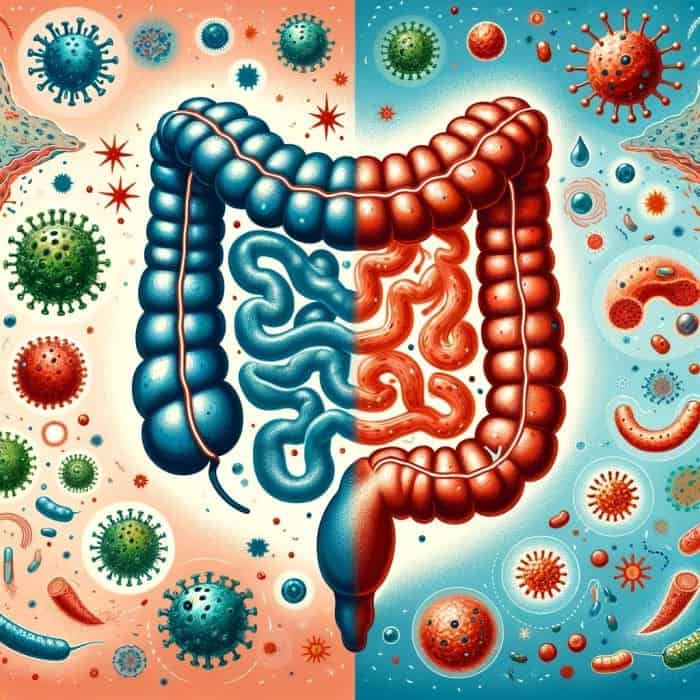
The various functions gut bacteria can have in health and disease have been shown by research in recent years, but what about the contributions of viruses, which, like bacteria, live permanently inside the human intestine? According to recent studies, abnormalities in the intestine’s virome, or viral community, may encourage inflammatory bowel disease (IBD).
- Chronic intestinal inflammation is a hallmark of IBD, which also includes Crohn’s disease and ulcerative colitis.
- Genetics, an overactive immune system, and environmental triggers are thought to be the primary causes of IBD. IBD causes changes to the fecal virome, suggesting that viruses may be involved in developing these diseases.
- Researchers discovered that viruses in a normal intestine had anti-inflammatory properties and contributed to a healthy gut when they isolated viruses from patients’ colon surgery tissue.
- In contrast, viruses found in the inflamed intestines of IBD patients induced inflammation. For their research to be applied in future research and clinical studies, the team classified the viruses specific to patients with IBD.
- The intestinal virome is formed at birth, changes throughout life, and is abundant with known viruses and what is currently unknown as “dark matter“.
- Our discovery fills a critical functional gap that suggests that although our collective virome contributes significantly to human health when disturbed, it can cause inflammation in IBD and potentially many other disorders.
Patients with IBD may benefit from treatments employing the virome, such as targeted virus eradication using vaccinations, antiviral drugs, or virome transfers, similar to fecal transfers, and replacing disease-causing intestinal viruses with healthy ones.
7. According to a recent study, HIV infection creates a “memory” in cells, the reason behind comorbidity in HIV-positive individuals (USA, Nov 2022)
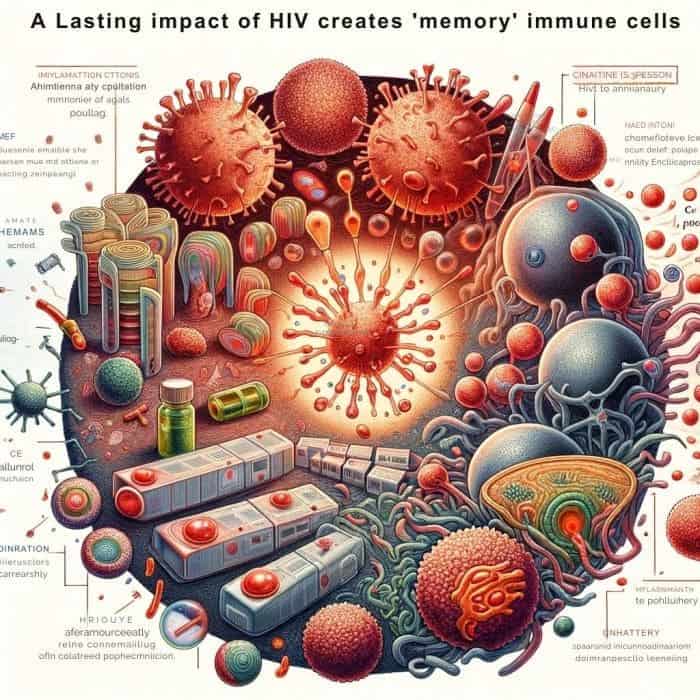
The research demonstrates how an HIV protein permanently changes immune cells, causing them to respond to other viruses. Immune cells exposed to the protein activate genes linked to inflammation, turning on or becoming expressed even after the HIV protein has left the cells.
- The research team carried out vitro human immune cell isolation and exposure to the HIV protein Nef.
- The amount of Nef that was delivered to the cells is comparable to the amount that is present in approximately 50% of HIV-positive individuals taking antiretrovirals whose HIV load is undetectable.
- After some time, the scientists added a bacterial toxin to cause the Nef-exposed cells to mount an immunological response.
- The cells exposed to Nef produced more inflammatory cytokinesWhat is cytokines?Cytokines are proteins released by cells that act as signaling molecules to regulate immunity, inflammation, and blood cell production. than cells not exposed to the HIV protein.
- The scientists discovered pro-inflammatory genes that were in a state of readiness to be produced due to the Nef exposure when they compared the genes from Nef-exposed cells with the genes of the cells not exposed to Nef.
- The final outcome depends on how long this memory lasts, and extended memory may be the cause of chronic inflammatory diseases like HIV infection or lengthy COVID.
- The results of this study may contribute to understanding why some comorbidities endure after COVID-19 and other viral infections.
This study emphasizes how crucial it is for doctors and patients to understand that suppressing or even curing HIV does not make these risky comorbidities go away. Researchers should keep looking for possible therapeutic targets that can lower inflammation and comorbidities in HIV-infected patients. Patients and their doctors should continue to discuss approaches to minimize inflammation.
8. Researchers discover new asthma and food allergy treatments (USA, Nov 2022)
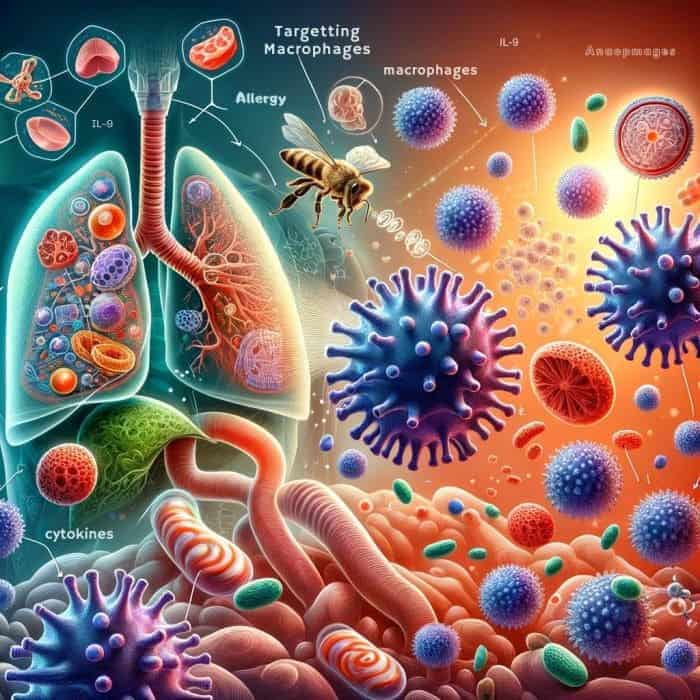
Asthma, which is brought on by allergen-induced lung inflammation, affects millions of children and adults in the US. The development of inflammation depends on the ability of cells to communicate with one another, which happens when molecules called cytokines are released. Interleukin-9What is Interleukin-9?Interleukin-9 (IL-9) is a cytokine involved in immune responses, such as allergy and asthma. (IL-9) is one of these cytokines identified in people with asthma and food allergies. However, it is unknown how IL-9 causes inflammation.
- This study identifies the lung macrophage as one of the cell types that IL-9 mostly targets.
- They discovered that the macrophage is essential for IL-9 action in the allergic lung and that allergic lung inflammation decreased when the IL-9 receptor was lacking.
- They also identified enzymes and other cytokines necessary for the emergence of allergic inflammation. They described downstream effectors of IL-9 in the macrophage. They discovered a relationship between IL-9 and the downstream effectors and the diagnosis of asthma in patients.
- This research makes major strides in the understanding of allergic lung inflammation.
With the help of this knowledge, we can examine the macrophage populations in more detail and see whether there is a way to treat asthma and other lung inflammations using macrophage populations as prospective therapeutic targets.
9. According to new research, RNA exosomes are essential for the growth of B cells (USA, June 2022)
Trichohepatoenteric syndrome (THES), a rare disorder associated with RNA exosome dysfunction, is characterized by a high prevalence of B-cell immunodeficiency and recurrent infections. The genetic cause of THES is not understood. However, it is linked to mutations in the exosome-encoding genes SKIV2LWhat is SKIV2L?SKIV2L is a gene that encodes a protein involved in RNA processing and is linked to certain genetic disorders like Trichohepatoenteric syndrome. and TTC37What is TTC37?TTC37 is a gene that encodes a protein involved in RNA processing and is associated with Trichohepatoenteric syndrome, a rare genetic disorder..
- The researchers examined a THES patient who had this mutation to better comprehend the function of SKIV2L in THES.
- This patient had a severely low blood count of B cells in addition to the typical clinical features of THES, a multi-organ disorder with symptoms such as small size at birth, uncontrollable diarrhea, distinctive “woolly” hair, and liver diseases.
- The SKIV2L gene was removed from bone marrow stem cells, which produce B cells, to create mice.
- Further investigation revealed that the B cells were absent from the animals‘ B-cell pools due to a crucial step in their formation, in which progenitor cells randomly recombine genetic material to produce a diversified B-cell pool.
- Further research revealed that B-cell insufficiency is also caused by mutations in other RNA exosome components.
- Because of these alterations render RNA exosomes useless, leading cells to retain specific types of RNA, especially those that don’t code for proteins.
- When overloaded with non-coding RNA, B-cell progenitors cannot develop into functional B cells.
- Together, the results imply that THES may be treated by a bone marrow transplant, which would substitute healthy B-cell progenitors for defective ones with a genetic mutation.
According to the study, hyperactive B cells, a major factor in autoimmune illnesses like lupus, may provide a new target for a treatment called SKIV2L. It may now be feasible to regulate the number of B cells, reducing the severity of the autoimmune response by decreasing the function of this gene.
10. New research shows how oral bacteria undermine defenses against viral expansion (USA, Jan 2022)
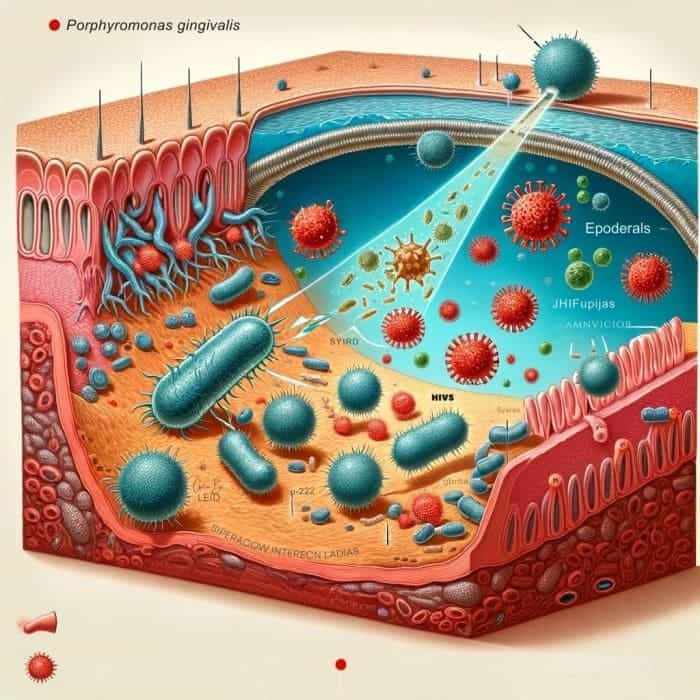
The oral bacteria Porphyromonas gingivalis decreases the generation and potency of a family of proteins known as interferon lambdas produced by epithelial cells in the mouth and plays a vital role in protecting humans from viral infection.
- The investigations discovered a specific pathogenic bacterial species, P. gingivalis, that causes periodontal disease and can significantly increase vulnerability to viral infection while entirely suppressing interferon production.
- These naturally occurring dental plaque bacteria are essential for controlling antiviral reactions.
- For viruses that affect the digestive system and lungs, such as SARS-CoV-2What is SARS-CoV-2?SARS-CoV-2 is the virus responsible for COVID-19, causing a global pandemic starting in 2019., HIV, herpes simplex, and cancer-causing viruses like human papillomavirus (HPV), the mouth is frequently a point of entry.
- Periodontal disease is brought on by the widespread oral bacterium P. gingivalis, which is also related to rheumatoid arthritis and Alzheimer’s disease. Recent clinical investigations have demonstrated how immune suppression in periodontitis patients can increase vulnerability to HPV, HIV, and herpes simplex.
- Researchers may develop treatment strategies to boost such protection due to a better understanding of how interferons provide all-encompassing antiviral protection and activate antiviral genes to protect humans against viruses. P. gingivalis also degrades interferon-mediated protection.
P. gingivalis has been linked to many other illnesses and ailments, including rheumatoid arthritis, Alzheimer’s disease, and esophageal cancer, according to this research. The research has extensive implications for host defenses against viral infections infecting mucosal surfaces and oral health.
11. Researchers successfully identify LAG3’s first crystal structure (USA, June 2022)
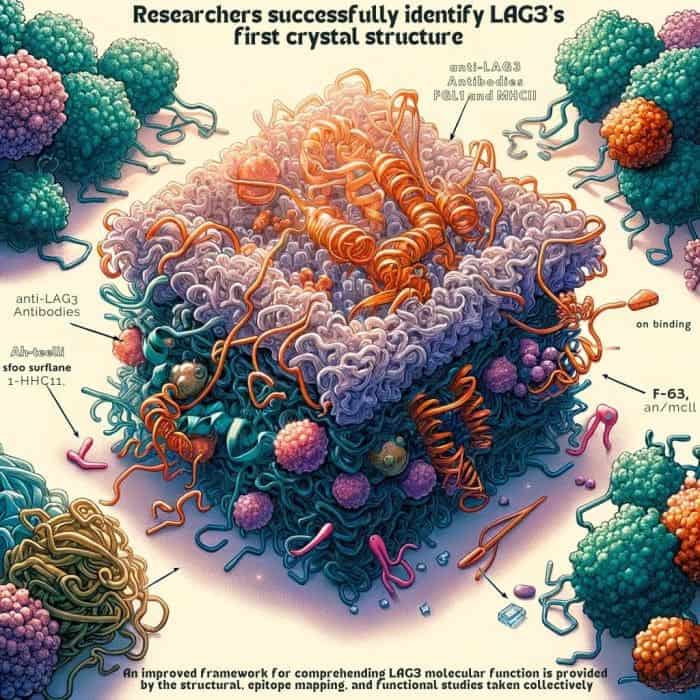
Despite this therapeutic advance, nothing is known about the LAG3What is LAG3?LAG3 is a protein involved in regulating immune responses, particularly in cancer and infection control. protein’s structure. LAG3-based medications must be designed “in the dark“, utilizing ineffective screening techniques since they lack a three-dimensional structure.
- Researchers have uncovered LAG3’s structural structure and its interactions with chemicals made by cancer cells.
- The group employed X-ray crystallography to “see” the LAG3 protein’s structure with almost atomic precision.
- The researchers also mapped the areas of LAG3 that reacted with the anti-LAG3What is anti-LAG3?Anti-LAG3 refers to agents or antibodies that target the LAG3 protein to modulate immune responses, often used in cancer immunotherapy. antibodies and the signaling molecules FGL1What is FGL1?FGL1, or Fibrinogen-Like Protein 1, is a protein that can inhibit immune responses, particularly in the context of cancer and liver diseases. and MHCIIWhat is MHCII?MHCII, or Major Histocompatibility Complex class II, is a group of proteins on cell surfaces important for initiating immune responses by presenting antigens to certain immune cells..
- With the help of this knowledge, they were able to identify the best antibody binding locations for inhibiting LAG3 activity.
- The researchers’ observations led them to conclude that LAG3 and FGL1 structural interactions restrict T-cell activity.
- They discovered that when the two molecules connect, LAG3 clusters on the surface of T cells. They speculate that this may help LAG3 exert its inhibitory function by preventing the T cells from correctly detecting tumor cells.
- The merged data provide several significant new understandings regarding the three-dimensional structure of LAG3 and its interactions with other molecules.
An improved framework for comprehending LAG3 molecular function is provided by the structural, epitope mapping, and functional studies taken collectively. Future therapeutic strategies that are more precisely focused could result from these discoveries.
12. Scientists claim that obesity is a dangerous immune interpretation of one’s body (Germany, March 2022)
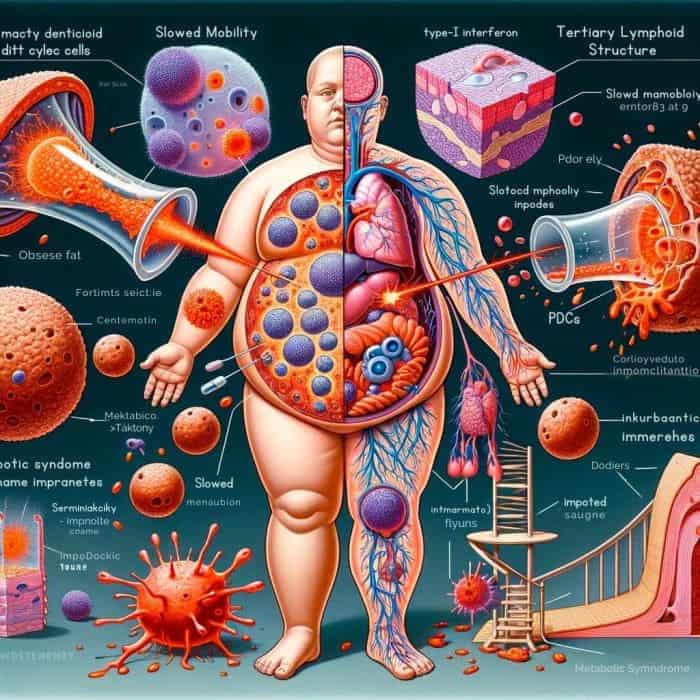
The progression of this illness is determined by immunological processes. In a recent study, a team of LMU demonstrated that even a three-week high-calorie diet significantly negatively impacts the immune system.
- The visceral adipose tissue starts to assemble Plasmacytoid dendritic cellsWhat is Plasmacytoid dendritic cells?Plasmacytoid dendritic cells are a type of immune cell known for producing large amounts of type I interferons, crucial in antiviral responses. (pDCs), a specific subset of immune cells.
- Internal organs are protected by this adipose tissue, which is found inside the abdomen. Small immune cell clusters form tertiary lymphoid structures inside this fat because of a high-calorie diet, triggering fatal immune reactions.
- These pDCs in visceral fat now constantly emit type-I interferon and are in a state of alarm.
- Normally, this interferon helps to control infections. Still, in this case, it causes metabolic syndrome, which results in a slowdown in metabolism and an increase in inflammatory markers.
- Weight gain is decreased, and the metabolic state noticeably improves when the migration of pDCs into the fat is blocked.
The findings of this study, which was conducted in association with Harvard Medical School in Boston, may help develop fresh strategies for treating metabolic syndrome.
13. Research findings might improve cancer immunotherapy (USA, May 2022)
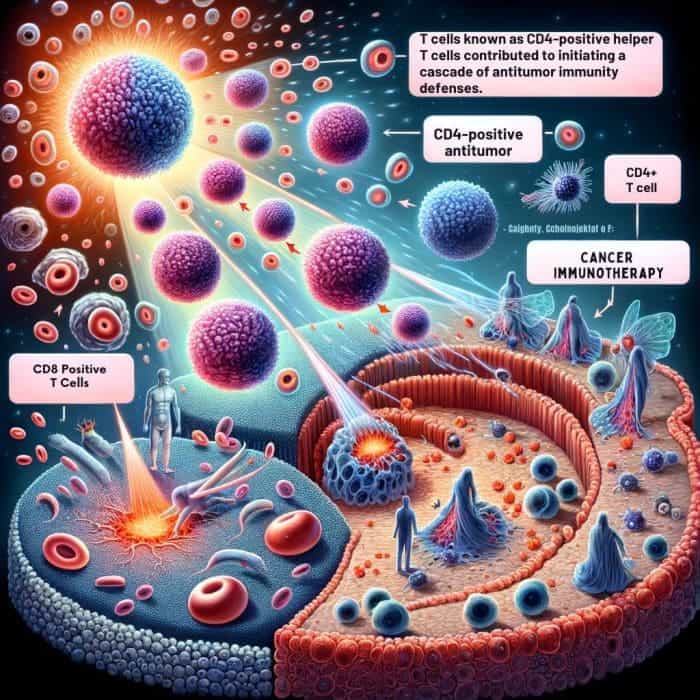
An immune system component of white blood cells previously only recognized as a supporter appears to be the driving force behind the body’s defenses against cancerous tumors. The finding might improve cancer immunotherapy, a promising therapy targeting cancer cells with the body’s immune system rather than radiation.
Scientists discovered that a group of T cells known as CD4-positiveWhat is CD4-positive?CD4-positive refers to immune cells, mainly helper T cells, that have CD4 receptors and play a key role in coordinating the immune response. helper T cells contributed to initiating a cascade of antitumor immunity defenses that facilitates the better invasion of melanoma and breast cancer tumors by killer cells.
- The ability of killer cells to infiltrate melanoma and breast cancer tumors more effectively is due, in part, to a population of T cells known as CD4-positive helper T cells.
- T cells are a subset of white blood cells called lymphocytes, which circulate throughout the body through the lymphatic system.
- The two killer cells in the immune system are the CD8-positiveWhat is CD8-positive?CD8+ refers to immune cells, mainly cytotoxic T cells, that have CD8 receptors and are involved in directly attacking infected or cancerous cells. T cells and so-called “natural killer” cells. Both can harm cancerous cells as well as virally infected cells. Innate and natural killer cells are found throughout the body.
- Although they serve as the first line of defense in our immune system, they cannot independently identify certain antigens, such as toxins or other foreign substances in the body.
- The CD8+ T cells, which can recognize particular antigens, arrive after the natural killer cells begin to function. While the mechanisms of CD8+ T cells have been extensively studied and are used in modern immunotherapies, little is known about how to activate the antitumor activity of natural killer cells.
- Zhang’s team discovered proof that a specific subset of CD4-positive T cells known as tissue-resident memory T cells may be crucial in triggering those initial natural killer cell defense lines using genetic knockout mice experiments.
- Their research revealed that they were successful in treating breast and melanoma tumors. The CD4 T cells in this particular population were crucial in triggering the antitumor immune response.
- Together with the natural killer cells, the targeted CD4 T-cells enhanced the infiltration of other white blood cells, or lymphocytes, into the tumor, killing tumor cells and controlling tumor growth.
To create an efficient cancer immunotherapy, the researchers intend to conduct further research into this antitumor immunity’s precise cellular and molecular mechanisms. The objective is to create a potent cancer immunotherapy strategy that works for all patients with various types of cancer.
14. COVID-19 research confirms that nasal sprays will be necessary to thwart variants (USA, July 2022)
Researchers have examined the impact of mRNA vaccination and natural COVID-19 infection on the mucus lining of the airways, the site of viral attack.
- The most widely used vaccines are called “mRNA vaccines” because they are modeled after messenger ribonucleic acid, the vehicle for biological replication.
- The vaccine’s mRNA, however, is not a live virus. Instead, the molecule is artificially created in a lab to resemble an invader closely enough that the body can eventually distinguish it from the real thing.
- With these vaccines, “the message” seems to have largely been contained to the blood. According to the study, the vaccine significantly increases bloodstream activity while having a moderate or minimal effect on mucosal linings’ production of neutralizing antibodies.
- In recipients of mRNA vaccines and infected individuals, the omicron variant almost entirely evaded neutralization by mucosal antibodies.
- To stop the virus from entering our bodies, mRNA vaccination also failed to stimulate enough tissue-resident cellular immunity in the airways.
- Higher cellular and humoral immunity results from the nasal vaccine’s mucosal antigen boost to T and B cells’ pre-existing immune response-directing memory.
The following studies thus show that COVID-19 vaccinations will not be sufficient to stop the spread of the virus and its variants, even if they keep the majority of the population free from a serious illness.
15. Researchers found that COVID-19 booster increases the longevity of the antibody response (USA, Dec 2022)
According to researchers, a booster produced longer antibodies for all recipients, including those who have recovered from a COVID-19 infection.
- The latest research clarifies how mRNA boosters, including those from Pfizer and Moderna, influence the longevity of our COVID-19 antibodies.
- The researchers claim that a booster resulted in more durable antibodies for all recipients, including those who have recovered from a COVID-19 infection. Antibodies naturally decline after an infection or vaccination, but higher levels are considered more protective.
- Thus, more sustained immunity against severe COVID-19 would be anticipated from antibodies with a longer half-life. The evolution of the COVID-19 vaccines’ immune response.
- The COVID-19 vaccine from Pfizer produced antibodies after the initial vaccination series that rose more slowly and declined more quickly than those produced by the Moderna vaccine.
- According to that study’s findings, the Pfizer vaccine generated fewer antibodies in older recipients than it did in younger recipients. However, this wasn’t the case for Moderna, where age didn’t seem to be a factor.
This study adds to the research showing that boosters are crucial for COVID-19 community protection. Boosters clearly increase the protection provided by the primary series mRNA vaccines alone, even though only about half of the U. S. eligible for one has received one.
Conclusion
Therefore, this immunology news gives us a broad overview of the recent advancements in the field. Studies show the mechanisms COVID-19 affects the gut immune system, the creation of a synthetic vaccine that can be tested in a clinical trial, and the targeting of this signaling cascade holds a significant key to improving current cancer immunotherapies, the research demonstrates how an HIV protein permanently changes immune cells, causing them to respond to other viruses, various cancer immunotherapeutic approaches, the role of mRNA vaccines and its immunization strategy. Through these scientific interventions and discoveries, we look forward to more interesting findings in 2023.