Discoveries in Immunology 2019: With every year, it is becoming clear that our immune system is significantly more complex than we previously realized. The interactions of different infections with immune cells are also very diverse.
One of the crucial discoveries in the year 2019 was that measles infection has another hidden danger – it can potentially wipe out previously made antibodies, thus making out immune cells “forget” previously encountered infections.
This discovery is especially relevant when so many refuse vaccinations. Moreover, immunizations can be helpful against autoimmune diseases.
As one study finds, eliciting responses to a particular bacterial structure can change the gut’s microbial balance and prevent excess inflammation. Another exciting piece of news is that there are previously unknown hereditary autoimmune diseases, such as CRIA syndrome.
Suggested Reading:
Explore 13 Different Shapes of Bacteria
Researchers have also made crucial discoveries that explain how the immune system fights viruses and bacteria.
Top Discoveries in Immunology 2019
Here are the top 10 recent discoveries in immunology for 2019:
RNAs can also lead an immune response: koalas have a type of RNA that prevents infection with koala retrovirus [USA-Australia-China, October 2019]

The first innovation in immunology in our list for 2019 comes from the world of Koalas. Koalas can be affected by several retroviruses that specifically infect their species. This retrovirus infection leads to the development of some cancers in these animals and increased susceptibility to infections.
Researchers have discovered a unique conserved innate immune response to these viruses in iconic Australian animals:
- A special type of RNA called Piwi-interacting RNAs (piRNA) are derived from the unprocessed transcripts of the retroviral genes.
- These piRNAs prevent the viral genes from transferring around the genome.
- The piRNAs act as “first responders,” preventing the viral insertion into the genome until more specific RNAs can be produced.
- This system is not foolproof; the virus can bypass and insert itself into the genome.
- The piRNA system seems to be conserved in koalas and is similar to systems in other animals, including insects.
As viruses have greatly influenced our evolution through history, the mechanisms existing in koalas are of particular interest to various researchers.
Suggested Reading:
What Do Koalas Eat?
![]()
Fighting death with death: injecting dying cells into tumors may trigger anticancer immunity [USA, June 2019]
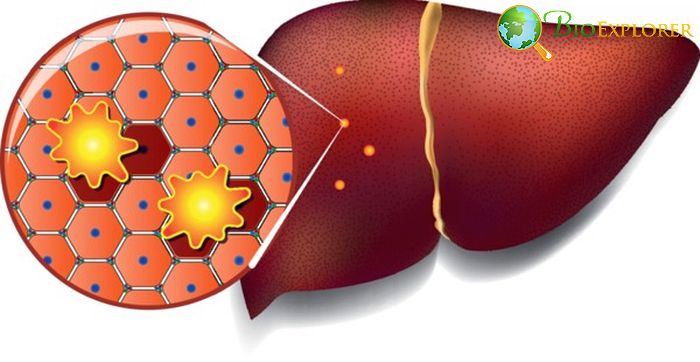
In normal circumstances, when the cell gets extensive damage for some reason or comes to the end of its life cycle, it undergoes apoptosis – programmed cell death.
Apoptosis is the opposite of necrosis – rapid death of the cell caused by external damage. Between these two opposites, there is a third category – necroptosis – when the immune system detects infected cells – and makes the cell kill itself.
This particular process combines features of both apoptosis and necrosis.
Necroptosis often stimulates a robust immune response, which led researchers to try to use necroptotic cells to attract the right kind of immune cells to cancer tumors:
- The research team has engineered cells with an activated RIPK3 protein.
- RIPK3 protein is known to activate a series of events that lead to cell destruction.
- The RIPK3-activated cells were injected into melanoma or adenocarcinoma tumors in mice.
- After the injection with engineered cells, the mouse tumors’ growth was slower than those not injected with engineered cells.
- When the treated tumors were dissected, it was found that the injection activated T-killer cells and increased processes associated with anti-tumor immunity.
- In another experiment, injecting adeno-associated viruses carrying the RIPK3 gene leads to tumor cell death and effective immune response.
This experiment can potentially become a foundation of a novel immunotherapy for cancer.
![]()
When immune cells fail to get fired up: chronic fatigue syndrome may be linked to changes in immune cells [USA, December 2019]
Myalgic encephalomyelitis has another name – chronic fatigue syndrome. Patients with this disease often fail to feel refreshed after sleeping, feel unexplained joint and muscle pain, and have cognitive task problems.
These symptoms become even worse after exercising. Unfortunately, there is no known cause or mechanism for this complex disease.
Researchers have looked into the state of immune cells in myalgic encephalitis (ME) patients in an attempt to understand the condition better:
- The researchers have isolated CD4+ (T helper cells) and CD8+ (T killer cells) from the ME patients and compared them to the healthy controls.
- They have found out that the activity of mitochondria in these immune cells is decreased.
- The immune cell’s mitochondria also had decreased glycolysis, one of the mechanisms of energy production in the cell.
- The impairments in the glycolysis level and the mitochondria activity in the immune cells were linked to the changes in the production of various immune-related proteins called cytokines.
This research provides an essential clue to the mechanism of the development of chronic fatigue syndrome.
![]()
Measles can make the immune cells forget: the new phenomenon of immune amnesia found [UK-Netherlands, October 2019]
Measles is a severe childhood disease associated with multiple complications. Currently, most countries offer vaccination for measles.
Sadly, the anti-vaccination movement has led to the resurgence of this disease, which, in turn, has sparked new research in the mechanisms of action of this infection.
A new study performed by an international research team has studied blood samples of unvaccinated children who contracted measles and also recreated measles infection in ferrets. They have found out:
- In the blood samples of 26 Netherlands children who contracted measles, specific immune memory cells carrying antibodies to the previously encountered infections have significantly decreased.
- In the ferrets, the quantity of new, naïve B – cells was reduced after measles infection.
- In the ferrets vaccinated against the flu before measles infection, the number of B memory cells carrying the antibodies against the flu decreased after being infected with measles.
- Consequently, ferrets that have encountered measles infection were susceptible to the re-infection with the flu strain they were previously vaccinated with.
Suggested Reading:
Albino Ferrets
These findings show the new side effect of measles, corroborating the necessity of vaccination against measles in early childhood.
![]()
Switching off autoimmunity: a switch responsible for the increase in energy production of immune cells driving autoimmune diseases found [USA-Japan, June 2019]

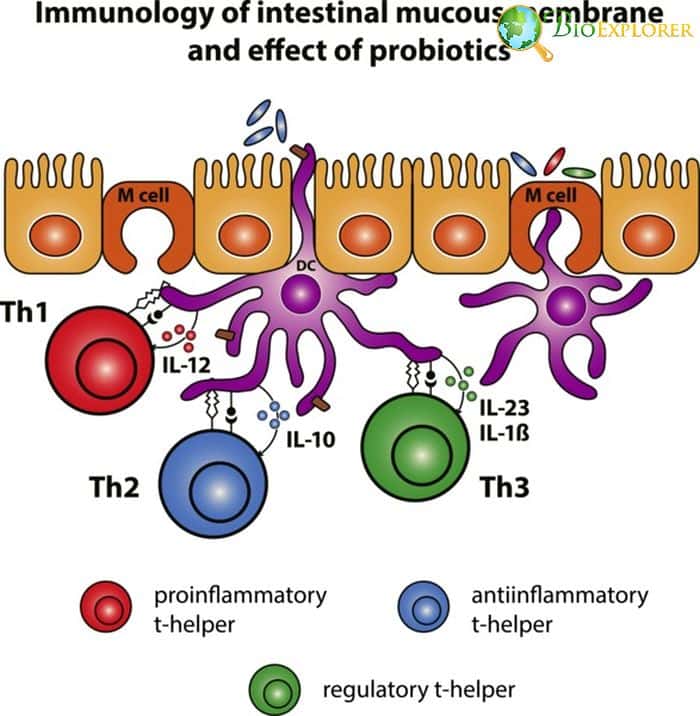
Autoimmune disorders are diseases caused by the increased pathological activity of several immune cells that attack the body’s cells instead of pathogens or damaged cells. The leading drivers of autoimmune disease are Th1 and Th17 cells. These cells are significantly dependent on glycolysis – a process of producing energy using carbohydrates.
The team led by Japanese researcher Michihito Kono aimed to find a way to decrease these cells’ activity by blocking glycolysis as their primary source of energy.
- It was known that glycolysis is initiated in part by activating an enzyme calcium/calmodulin-dependent protein kinase IV (CaMK4).
- T cells that had a disabled CaMK4 gene or that were exposed to a CaMK4 inhibitor had lower glycolysis rates compared to healthy cells.
- Additional tests have shown that CaMK4 interacts with another crucial enzyme, pyruvate kinase muscle isoenzyme 2 (PKM 2).
- If PKM2 was blocked, not only the level of glycolysis was decreased, the naïve T cells could not become Th4 cells or Th17 cells.
- Increased level of PKM2, in its turn, leads to the development of Th17 cells.
- In the autoimmune encephalomyelitis model, treatment with a compound that blocked PKM2 activity improved the disease symptoms.
These findings show a potential target for autoimmune disease treatment.
![]()
Frederick W. Alt Award for New Discoveries in Immunology was given to a scientist who discovered a new immune cell subset.
Shane Crotty has been awarded a Frederick W. Alt award from Cancer Research Institute for his extensive research on a subset of T cells.
- In 2009, Crotty discovered a transcription factor called Bcl9, which defines the differentiation of a specific T cell subset called follicular T helper cells (Tfh).
- Tfh cells are necessary for the development of specific centers called germinal centers. The B cells mutate, and the antibodies they produce mature.
- his research has expanded considerably, and Tfh cells were found to have a significant role in different diseases.
- Tfh is involved in anti-infectious immunity (particularly response to HIV infection), autoimmune diseases, heart disease, and allergy.
This field is still of considerable interest to specialists, and Dr.Shane Crotty is currently a professor at the La Jolla Institute for Immunology. Moreover, he is currently a T-cell expert at one of the consortia responsible for HIV vaccine development.
![]()
No wriggling in the gut: immunization against flagellin may protect from intestinal tract infections [USA, December 2019]
Immunization is usually reserved for protection against pathogenic infections. A recent study has shown that it may be a form of treatment for diseases linked to changes in the non-pathogenic microorganisms‘ communities living in our guts.
For instance, when a patient develops an inflammatory disease in the intestinal tract – metabolic syndrome, inflammatory colitis, inflammatory bowel disease (IBD) – the community in their intestinal tract also changes.
It was shown that the percentage of bacteria capable of movement and a unique structure called flagellum increases in patients with these diseases.
Researchers have decided to check if one could prevent the appearance of those bacteria in the first place, thus decreasing the level of inflammation:
- The team has created a model of inflammatory colitis (IC) in mice.
- Some mice participating in the experiment were receiving flagellin, a central component of the bacterial flagellum.
- The injections have led to the synthesis of anti-flagellin antibodies in mice.
- As a result, there was less flagellin in the feces of the immunized mice. The percentage of harmful bacteria in the gut decreased.
- The level of obesity in the injected mice was lower.
- Due to immunization with flagellin, the mice were partially protected from developing inflammatory colitis.
As the increased flagellin in feces was also observed in humans with metabolic and inflammatory diseases, this experiment shows that immunization against flagellin may be protective against these diseases in human patients.
![]()
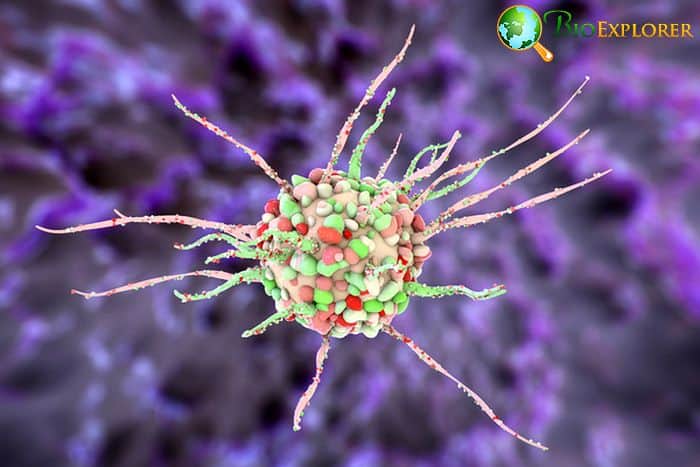
Differentiating the viruses: a study has revealed a crucial component of the immune response to viruses that can differentiate viral intruders [Australia, August 2019]
Discovery has shown that the immune system does not paint all viruses with the same brush and has a mechanism that allows the body to differentiate between them, depending on their mode of action.
- T-bet is a factor produced by follicular T helper cells (Tfh).
- T-bet is known to influence the fate of Tfh and the production of antibodies.
- A team of researchers decided to compare the T-bet level in the case of two infections: influenza virus and LCMV (causative agent of meningitis).
- Influenza infection leads to a moderate T- bet production.
- In the case of influenza, moderate levels of T-bet lead to repression of Tfh and activation of another T cell subset – Th1.
- LCMV infection leads to high production of T-bet.
- High production of T-bet leads to activation of both Tfh and Th1 cells.
- Different T-bet levels also influence the types and quantity of antibodies produced by another immune cell class – B cells.
These findings show that T-bet plays a crucial role in managing the response to different viruses, controlling which immune cells are involved, and the type and amount of antibodies produced. This knowledge can be crucial for developing better vaccines against viral infections.
![]()
New inheritable inflammatory disease discovered [Australia – USA, December 2019]
A group of diseases is caused by an abnormal, unbalanced inflammatory response generated by the immune system called autoinflammatory diseases.
Recently, a team of researchers from Walter and Eliza Hall Institute of Medical Research in Australia and the US NIH research center has encountered patients from three families who exhibited symptoms that could not be linked to any known disease.
- The patients complained of:
- Periodic fevers
- Severe pain in the abdomen
- Swollen lymph nodes
- Gastrointestinal problems
- Headaches
- Some patients also had an enlarged spleen and liver
- No tumor or infectious cause was found in these patients.
- Whole exome sequencing has revealed that all patients had mutations in the same gene – RIPK1.
- Experiments in mice with manipulated RIPK1 have shown that in normal conditions, RIPK1 regulates inflammation and necroptosis – a type of cell death caused by infection.
- If the RIPK1 gene has a mutation, the resulting protein cannot be adequately processed, which leads to imbalanced inflammation.
- Mice with two faulty copies of this gene die very early.
- Mice having only one copy tended to have high inflammatory responses to any trigger.
- The newly discovered syndrome was named CRIA syndrome.
At present, this new disease is not much known. The patients could be treated with many corticosteroids and other biological anti-inflammatory agents. Still, the success of the treatment at present is moderate.
![]()
Fighting infection is a community action: a specific process “fueling” the developing immune cells in response to Salmonella infection found [UK, August 2019]
When an infectious agent enters the body, it must produce new immune cells in response. The “production center” is located in the bone marrow. There, the future immune cells are surrounded by “support groups” – stromal cells.
A new role for these stromal cells was found recently.
- The mouse model noted that infection with Salmonella led to an increase in the so-called reactive oxygen species (ROS).
- The increase in ROS signals the presence of infection in the stromal cells in the bone marrow.
- In response, a particular protein called PI3K gets activated.
- P13K activation opens channels in both stromal and future immune cells.
- The stromal cells send their mitochondria into the young immune cells through these channels.
- An increase in mitochondria quantity means an increase in energy production, thus basically “powering up” the maturation of the immune cells.
- If this transfer of mitochondria is blocked, the colonization of bacteria can grow rapidly.
This discovery points to a significant event that determines the development of infection in the future.
![]()
Immunology research is crucial for multiple disciplines – cancer biology, endocrinology, vaccinology, and gastroenterology. Even fundamental research in immunology can have practical applications.
For instance, a series of studies devoted to T cell exhaustion programming and switch proteins involved in this process can hopefully inform a new cancer immunotherapy approach. There are other approaches aimed at destroying tumors: from the above idea to use dying cells to attract immune response to the new catalytic immunotherapy.
It is also essential to learn to suppress the immune system when it is overactive: for instance, with the help of the newly discovered type of immune cells that can suppress inflammation in the gut or by blocking a compound that can downplay the activity of immune killer cells.
Another important discovery contributes to our understanding of Ebola infection – that can potentially become a threat at any time, as a current news show.
As we see, immune system research and the development of new vaccines are crucial for the world’s survival in a time of an increasing incidence of new viral infections, autoimmune diseases, and chemotherapy-resistant cancer.
Let us hope breakthroughs will await us in the year 2020 as well.
![]()